Context
At Optimus SBR, we regularly keep an eye on public sector developments. In March, we discussed Ontario’s changing health care landscape, Ontario Health Teams (OHTs), and how organizations can respond. Since then, there have been several new developments which matter a lot for health and social system organizations.
First, the Premier’s Council on Improving Healthcare and Ending Hallway Medicine issued its second and final report, “A Healthy Ontario: Building a Sustainable Health Care System.”[1] While it comprises a set of recommendations and is not yet a policy, it gives some hints on the government’s direction, including potential changes to privacy and home care legislation, a focus on virtual care, and continued strong emphasis on the role of primary care in a more integrated health system. OHTs are clearly central to the thinking of the Council as well.
Second, following a flurry of activity leading up to the May 15th deadline to undertake the OHT Self-Assessment, the Ministry of Health (MOH) found over 150 Self-Assessment Forms (SAFs) on its proverbial front step, an overwhelming response. Finally, on July 18th, Minister Elliott and Deputy Angus announced via webinar the results of the process, through which 31 groups have been invited to proceed to the Full Application stage of the OHT process. Since then, a series of webinars have been made available to prospective groups on a wide variety of topics related to OHTs and the Full Application.
Why does all this matter? Because organizations need to figure out what a single fiscal and clinical accountability structure looks like for their patients and themselves in an OHT world, and how to work with others to get there. The MOH has made some significant decisions. As a result, for many organizations now, it’s decision time.
Ontario Health Teams and the Designation Process
As mentioned, the OHT process started with the SAFs. For reference, we have reproduced the MOH’s diagram from the OHT guidance document below:[2]
Figure 1: The Ontario Health Team Designation Process
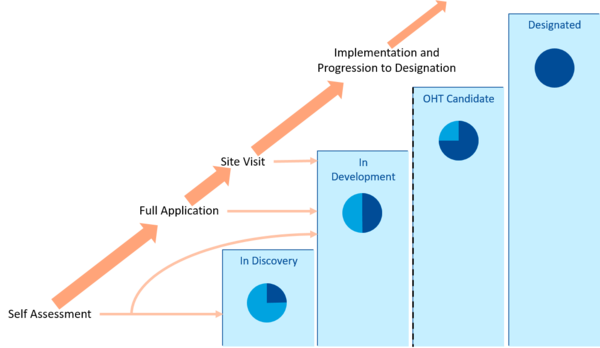
Source: Ministry of Health
Now that the MOH has completed its validation process for the 150-plus SAFs received, it has sorted the groups into ones that will:
-
- Proceed to Full Application (31 groups) – those with a “high level of readiness”;
- Be “In Development” (43 groups) – those that need “a bit more work” before they proceed to the Full Application;
- Be “Innovative Models” (9 groups) – a new category defined by the MOH which often addresses special populations; and
- Be “In Discovery” (70+) – those that are “encouraged to expand their partnerships and work with other local providers” to move forward.
During the webinar, the Minister alluded to another category not initially included – those that are “Innovative Models”. These SAF submissions outlined regional or provincial approaches that the MOH saw as worth exploring further for an OHT-driven health system.
There is still a long road ahead – Full Applications are due October 9th, and Ontario Health Team Candidates will be announced in the (presumably late) fall. There will also be a second round of self-assessments, with SAFs that will be due on December 4, 2019.[3]
Clearly, it’s a process meant to drive innovation and spread growth of good things currently happening in the system. When asked how many of the Full Application group would become Candidates, Deputy Angus said she hoped “they all will”, suggesting it is about reaching a standard, rather than a competition per se, as some have interpreted it. The long-term vision appears to be one where most providers in most communities will say “We are all OHTs now.” Naturally, organizations will want to control or at least influence their own destiny. But not everyone can lead.
It is also important to remember that for the successful Candidates, the real work starts from the fall onwards through “Year One”, for which the MOH has set a series of expectations, the most important of which is the group’s readiness to “receive an integrated funding envelope and enter into an Ontario Health Team accountability agreement”.[4] The MOH has also indicated that it may become a matchmaker of sorts, by asking groups to collaborate with additional providers and resubmit a joint SAF.
Decision Time
So, if you are one of the 31 groups that has been selected for Full Application, then well done! Less than 1 in 5 of the groups submitting SAFs made it to this stage. And if you are currently one of the 43 “In Development”, you are still in good company. For those that are now “In Discovery” – roughly 70 or more of you – or if you were not part of the Self-Assessment process at all, then you will likely have somewhat different decisions to make.
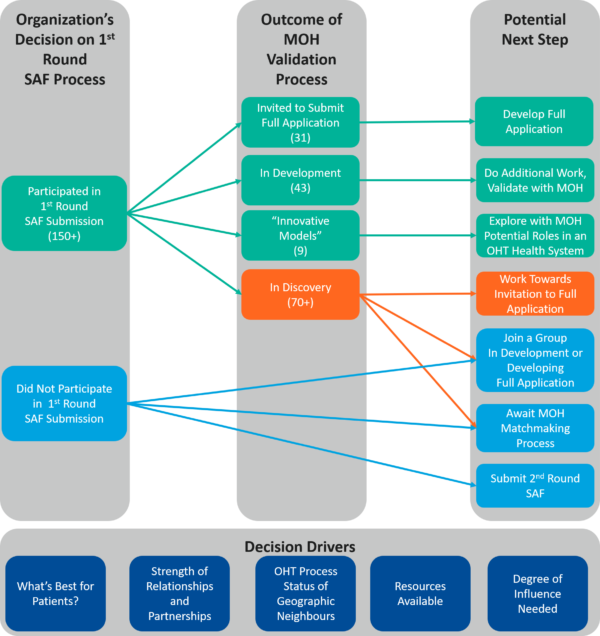
Going forward, it will be important to keep the momentum going, make decisions, and plan carefully. In Figure 2 below, we have sketched the paths available to prospective OHT groups. While organizations – even those invited with their partners to the Full Application process – can always pause or stop their participation, the general assumption here is that organizations will move forward. Partnerships can change too. In the meantime, we have sketched the pathways in terms of participation in the SAF process and the outcome of the MOH’s validation process.
Figure 2: Pathways for Organizations Considering Ontario Health Team Designation
Considerations by Pathway
Invited to Submit Full Application
The next step for organizations in this group is pretty straightforward: develop and submit the Full Application by October 9th, 2019. With summer vacations and an inevitably busy September, this doesn’t leave much time. We think you may need to:
1. Reconfirm Commitment in the Group: The SAF process happened quickly – your organization may have gone from first learning about OHTs to making commitments about them in a matter of weeks. Your Board or others’ might even view this early success with some trepidation. So, now that you are taking a step closer to OHT designation status, you will likely want to reconfirm the level of commitment among the organizations in the group.
Putting together an OHT can be challenging, and you don’t want partners getting cold feet in early October, so there are some questions to consider: Is the level of trust great enough to overcome the challenges ahead, or is a more formal arrangement needed? Do you have a good track record of working together, or was the SAF process a bit of trial by fire? In short, is the commitment there in the group to proceed?
2. Build Out Decision-Making Processes Further: With more time to prepare for the Full Application than the SAF, and commitments to the MOH escalating, Boards may demand more involvement and clarity in decision making. Reaching consensus or agreeing on how decisions will be made can be challenging, but challenges not dealt with now will only surface or cause strained relationships and halt progress later. Ask yourself, for the Full Application and the longer term, how will decisions get made quickly and effectively? You will likely need to set up some of these processes, or at the very least agree on working understandings quickly.
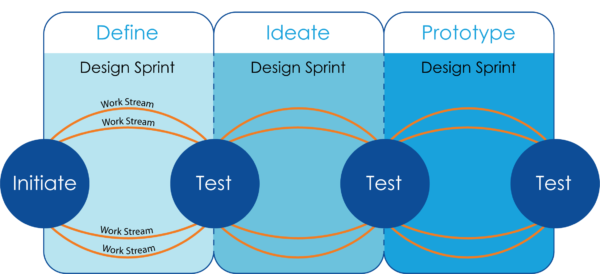
3. Design How You Will Design Year 1 Programs, With the Patient at the Centre: No, that’s not a typo. You will need to design what your Year 1 programs will look like, but you’ll also need to design how you will design them. You’ll need to think about how you can improve care for your population of choice, and what is in and out of scope for Year 1. But after that, use design sprints and an iterative program and function design (e.g., intake and referral, care delivery, hand-offs) to tackle the biggest challenges, and create solutions that transform care. This will help you identify patients, gauge impact, and hit the ground running when you scale up. And patients need to be kept at the centre and involved in the design – how will they play a part in the experimentation that happens?
4. Divide and Conquer on Other Areas: This group will also encounter the thorny questions first: governance, funding allocation from a common envelope, contract and volume management, and how to best use or combine available back office functions. You will likely need separate work streams working in parallel with the Year 1 programs work to move this all forward. Treat it like a project, with appropriate project management support, to keep it on track. Additionally, there may be work internal to your organization required to meet OHT requirements – such as addressing any pressing financial or operating challenges that limit your ability to invest resources in redesigning care.
5. Develop the Full Application: A robust application will take work, as it will be much longer than the SAF; while many aspects build on the SAF, others require significant system redesign efforts. Some of the elements that may require a bit more work than others include creating detailed plans for:
-
- Providing fully integrated care and the whole continuum of services;
- Providing seamless and effective care transitions;
- Providing 24/7 access to coordination of care, especially for ‘patients who require higher-intensity care’ (including the activities in and out of scope, how it will be done, by who, how many resources, etc.);
- Providing more virtual care, and giving patients digital access to their own health info; and enabling digital information sharing among team members.
For these aspects and others, the MOH is looking for specifics and evidence that what you propose locally will be effective and perhaps scalable to the rest of the province.
In Development
This group, as the MOH puts it, has “a bit more work” to do before the Full Application. This may mean a few tweaks or may be more involved. In any event, we think the next steps for this group are:
1. Listen and Reflect: It’s important to understand where your group needs to improve. Once you have feedback from the MOH on your SAF submission, take time to reflect honestly:
- Do you have in place the readiness components (e.g., working relationships, capability, capacity, leadership, successful track record, etc.) you need?
- Did you successfully convey the messages/ideas you intended?
- How can you differentiate better, either generally or from a group of your neighbours that are among the 31 groups listed above?
- Are there opportunities to collaborate with other partners or other groups?
2. Develop your Relationships: The self-assessment process helped organizations build stronger relationships with other providers in their communities and consider new working relationships. In our work, we continually see how good relationships facilitate more collaborative care planning. Yet we are often surprised to see health service providers in the same area that have never met before. The MOH may want the group to expand (as the OHT Guidance Document says: “Note: Where appropriate, groups may be asked to collaborate with additional providers to re-submit a joint Self-Assessment.”). Your group may need to work with other organizations beyond those initially envisioned.
3. Address Readiness Gaps: Core to the work required to move from In Development to Full Application is achieving the level of readiness required to proceed to Full Application. Leverage what you heard while listening and reflecting, and prioritize the most important gaps to be addressed. This may include identifying new partners to broaden the care continuum represented by partners, engaging your community and patients/clients to assist with co-design efforts, increasing your understanding of Year 1 target patient/client populations, improving organizational finances and operations, and/or creating digital health capabilities.
Innovative Models
A new category emerged from the SAF process when the MOH indicated that several groups had presented innovative models that would be considered. These models went beyond some of the original concepts around OHTs, and include support models that are provincial or cover broader regions than typical OHT geographies. The MOH will be working directly with these groups to further explore their potential role in an OHT-based health system. Organizations focused on providing care for special populations or providing specialized services with broader catchment areas will have more flexible options. While not necessarily needing to join an OHT, they will need to relate and work well within an OHT-based health system.
The next steps for these groups is less formally defined, but we would suggest:
1. Define/Refine Your Vision and Scope: Ensure the vision for the innovative model is clear, and that participating parties agree with what the model seeks to achieve. Similarly, refine the proposed innovative model scope to an approach compatible with service delivery across multiple OHT geographies and the proposed role of Ontario Health.
2. Segment Design Efforts by Function: As you begin designing the model, identify the enabling functions required beyond direct service delivery. Should the model have centralized intake and referral? Does it require care coordination/navigation? How will information be shared between model partners and with OHTs delivering less specialized care to the same patients/clients? Once all required functions have been determined, identify design dependencies – does Function A need to be designed before Function B? Consider grouping similar functions (or functions that require similar skills to design) together into work streams.
3. Design Your Model in Sprints: Take an iterative approach to design that allows several work streams to proceed concurrently. This involves prototyping initial functional designs, testing the design, then refining and iterating repeatedly until the base functions and associated services, roles and responsibilities have been defined.
In Discovery or Did Not Participate in a 1st Round SAF Submission
As Figure 2 suggests, the options for organizations in this group can go in a number of different directions. As we suggest for groups In Development, take time to listen, reflect, and develop relationships. With one exception, the options for a group that is In Discovery and for organizations that did not participate in the first round of SAF submissions are the same. We’ve outlined some pros, cons and next steps for the options below.
Table 1: Options for Groups In Discovery or Organizations that Did Not Participate in First Round
Option Pros Cons Next Steps Work Towards Invitation to Full Application
(assumes a SAF was submitted)• Ability to control OHT design and priority initiatives and target populations • Significant work is likely needed to move from In Discovery to Full Application invitation • Identify gaps and model components to be addressed or strengthened
• Consider reaching out to the MOH for feedback
• Ask OHTs proceeding to Full Application to share SAF to learn from their proposed approachesJoin a Group In Development or Developing Full Application • Requires fewer resources than forging ahead with present group • Less control and influence in the way the OHT is designed • Identify the proposed OHTs who you share the most patients/clients with and discuss the opportunity and timing for joining No previous submission: Submit 2nd Round SAF
(December 4, 2019)• Greater control over how your organization partners with others to become a potential OHT • With over 150 SAFs submitted to date, finding partners not already participating in an OHT in your geographical location may be difficult • Identify potential OHT partners and begin SAF process early to allow time to develop relationships and design a thoughtful OHT approach Await MOH Matchmaking Process • Opportunity to wait, watch, and learn from others going through the process
• Effort not required at this stage• Likely less control over the organization’s destiny and role later on • N/A So far, however, the process is pushing local health service providers to talk more, plan with other providers that aren’t the “usual suspects”, and think big about ways to improve care. That’s some progress towards integration and innovation. In the meantime, the road ahead may be a bit bumpy.Given that OHTs are new and appear to have a lot of freedom to chart their direction, they require a leap of faith. Change is coming quickly, many elements of the big picture and the details still need to be worked out, and there isn’t a lot of time to prepare.
Optimus SBR’s Health Care Practice
Optimus SBR is an implementation-focused firm that specializes in turning policy into action. Our team has significant experience working with major health care stakeholders, including the MOH, hospitals, LHINs, home and community care, and community health service providers. We partner to create new models of care, facilitate decision making, assist with implementation and integration efforts, and develop proposals for government approval. With our real world health care integration experience, we help organizations get done what isn’t.
We have a wide range of service offerings and can support your OHT development in a number of ways, including:
- Facilitation: Experienced, neutral, third party facilitators that can ask the tough and thought-provoking questions as you work through the “thorny issues”.
- Business Case Development: Teams that know how to develop a compelling business case and help you work out the kinks along the way.
- Model of Care Design and Implementation: Knowledgeable and experienced health care experts who can guide and inform development and implementation efforts.
- Project Management and Action Planning: Planners and project managers that help your team clearly set a roadmap, milestones, and accountabilities, and can help give the plan the attention it needs.
If you found this helpful, give us a call, or send us a note.
Brad Ferguson, SVP, Industries and Government Practice
Brad.Ferguson@optimusssbr.com
416.649.9184David Lynch, Principal
David.Lynch@optimussbr.comJason Huehn, Senior Manager
Jason.Huehn@optimussbr.comNathan Duyck, Manager
Nathan.Duyck@optimussbr.com[1] Premier’s Council on Improving Healthcare and Ending Hallway Medicine (2019). A Healthy Ontario: Building a Sustainable Health Care System. Toronto: Queen’s Printer. [online: web] URL: https://files.ontario.ca/moh-healthy-ontario-building-sustainable-health-care-en-2019-06-25.pdf.
[2] Ministry of Health (2019). Ontario Health Teams: Guidance for Health Care Providers and Organizations. Toronto: Queen’s Printer. [online: web] URL: http://health.gov.on.ca/en/pro/programs/connectedcare/oht/docs/guidance_doc_en.pdf, p. 12.
[3] Ministry of Health and Ministry of Long-Term Care (2019). Become an Ontario Health Team. Accessed July 24, 2019. [online: web] URL: http://health.gov.on.ca/en/pro/programs/connectedcare/oht/#readiness.
[4] Ibid., p. 10.

Optimus SBR Celebrates 6 Consecutive Wins as 2024 Best Workplaces™ in Professional Services
Our commitment to a people-first approach has been central to being recognized in 2024 for the sixth time as one of the Best Workplaces™ in Professional Services and the key to our overall success.

12 Best Practices to Increase Cross-Team Collaboration and Enhance Organizational Alignment
Enhancing cross-team collaboration drives innovation, optimizes resources, improves overall performance, and ensures every part of your organization works toward the same goals.

Enhancing Your Data Strategy for Success: The Power of Metadata
Metadata goes beyond just aiding in data retrieval. It ensures your data is secure, compliant and, most importantly, understood consistently by everyone in the organization.

Optimizing Language Translation Strategies: Beyond Compliance to Enhanced Operational Efficiency
The introduction of Quebec’s Bill 96 in Canada underscores the necessity for comprehensive translation strategies. Integrating machine translation technologies helps meet regulatory requirements while enhancing translation speed, cost efficiency, and operational effectiveness.

How to Manage Gen Z: 16 Strategies to Engage and Retain Young Talent
These practical strategies lead to a workplace that is better aligned with the values and expectations of Gen Z employees, ensuring that your efforts to attract and retain Gen Z talent are both successful and sustainable.

How to Measure the Success of Learning and Development: 12 Important Metrics to Evaluate
Quantifying the success of L&D training programs can be challenging. Learn about selecting and measuring the right metrics to determine whether your training efforts are truly making an impact.